Table of Content
Coding and OASIS were derived to develop an effective score to show through data the condition of the patient at the time of assessment. To avoid LUPA there needed to be more than 4 and to stay under the radar, less than 20 therapy visits. Anything in between would not normally raise many questions. Naturally, many home health agencies and therapists would then provide as much therapy as possible in order to increase revenue for both the agency and therapist.
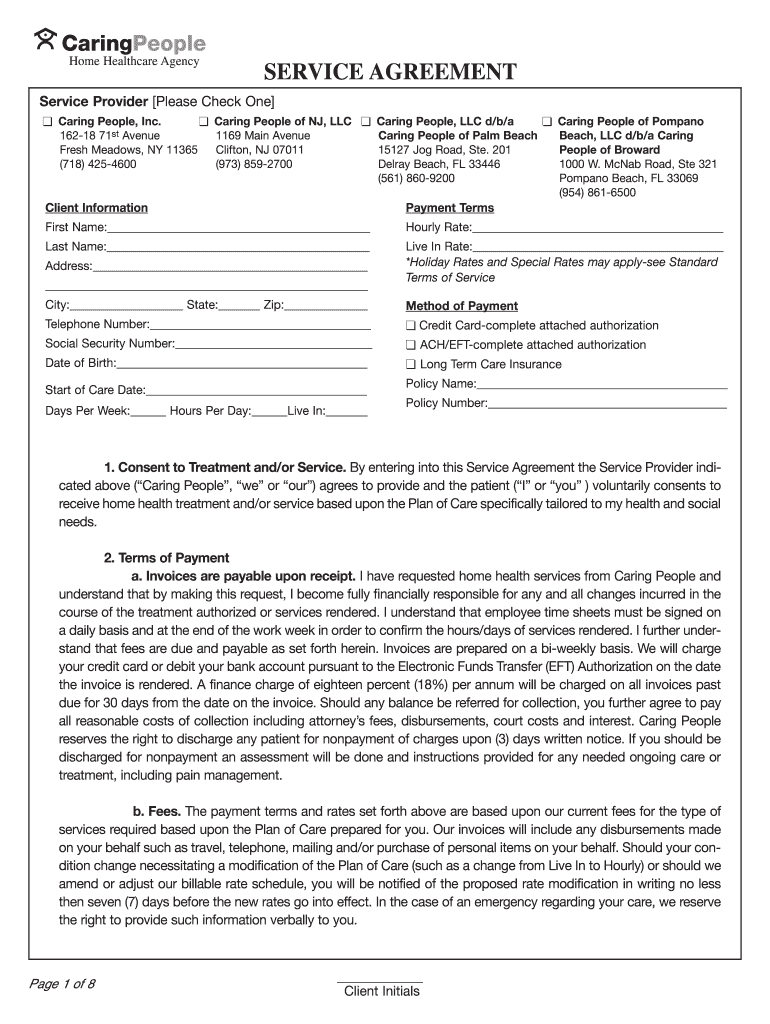
If you do not agree to the terms and conditions, you may not access or use the software. Instead, you must click below on the button labeled "I DO NOT ACCEPT" and exit from this computer screen. Home Care Answers takes the guesswork out of what you expect to receive for Medicare reimbursement.
Home Health Patient-Driven Groupings Model
With the number of changes in store, inevitably some agencies will contest specific aspects of PDGM’s new requirements. In the past, CMS has already suggested PDGM isn’t budget neutral and is over-paying home health providers. Following 2020, CMS concluded that 2020 base payments were set 6% higher than they should have been. Going into 2020, nearly half of home health agencies planned to decrease therapy utilization, according to a mid-2019 survey conducted by NAHC ahead of PDGM implementation. The general concepts of medicare secondary payer billing will remain the same under PDGM.

Make sure summaries and narratives tie to OASIS and Plan of Care . Our view is that they can achieve desired results with more efficient use of time and resources. Questionable Encounters refer specifically to the primary diagnosis on the claim. Diagnosis codes that would qualify as a QE in the primary diagnosis spot can be listed as a subsequent diagnosis on the claim. The main concept here is that these diagnoses represent a symptom of the patient’s condition but on their own do not constitute home health eligibility. PDGM is leading to shifts in the way many agencies operate so they can maximize reimbursements under the new model.
PDGM Best Practices: Ensure Smooth Claims Processing in Home Health
Home Care Answers provides individual reports for each chart we review along with data compiliation to show data at any level you want. We can show data by clinician also with custom date ranges. Data Drives Decisions, but Great Data Drives Great Decisions. Providers quickly went from questioning the frequency of therapy visits to going back to giving the therapist control of determining frequency due to COVID-19.
Therefore, with PDGM therapy was removed as a component of the reimbursement calculation. Home Health Agencies now use a combination of diagnosis coding and OASIS data to determine the reimbursement rate. Other components used in the calculation is episode timing (early/late), referral source (institutional/community)- which institutional results in an automatic 10% increase in reimbursement. With all of this data together, a reimbursement amount is determined- independent of the amount of visits/therapy needed.
NAVIGATING THE INTRACACIES OF PREPARATION, CHALLENGES, & UNDERSTANDING PDGM
Providers who have successfully navigated PDGM and are seeing positive returns from the updated payment model will actively seek agencies who were not as prepared for PDGM and are suffering from its effects. This event explores the strategies for deals, investments and transactions in the home health, home care, hospice and palliative care space. Yet because of the COVID-19 pandemic, any major recalibrations or corrections to PDGM’s foundation have, so far, been delayed, according to National Association for Home Care & Hospice President William A. Dombi. That could begin to change later in 2022, when CMS is gearing up to release its proposed payment rule for 2023.
Grouping to determine the HIPPS code used for payment will occur in Medicare systems and the submitted HIPPS code on the claim will be replaced with the system-calculated code. Home Care Answers helps many agencies across the country with varying census from 15 patients to over 500. We provide a complimentary chart audit to create enough data to give some guidance. Almost without fail, one of our first suggestions is improving documentation. While it’s likely true that PDGM did have some influence on therapy utilization, finding out how much is nearly unquantifiable.
HOME HEALTH AGENCIES ADAPTING TO PDGM
Many home health advocates do not like the idea of creating a behavioral adjustment before new regulations take effect. + Behavioral Health ∨+ Addiction & Substance Use Disorders ∨+ Children, Youth & Families ∨+ Resources ∨Count on Relias to support your journey toward better care and financial outcomes with reliable thought leadership and expert advice. Sign up for our newsletter to receive latest news, offers and alerts. First Position - a numeric value representing a combination of the referral source and the period timing . Optional reporting of new Occurrence Codes 61 and 62 identifies the admission source. This license will terminate upon notice to you if you violate the terms of this license.
Within the current system, home health providers receive a LUPA claim for providing 4 or less visits over 60-day care episodes within any category of patient delivered care. Providers then in turn only get a standardized per-visit payment, no matter the cause for fewer recorded visits. The new PDGM rules will effectively transform that universal four-or-fewer rule and morphs it into 216 differing scenarios. In consequence, estimated LUPA rates are expected to fall from 8% to 7.1% once PDGM takes effect, with scattered predictions that they may increase.
The intention is to deliver the same amount of care to achieve optimal outcomes, but do within a defined per patient budget. Categorization of 30-day periods into a payment category or Home Health Resource Group based on 432 case-mix groups that are determined by a combination of admission source and timing, clinical grouping, functional impairment level, and comorbidity adjustment. PDGM will undoubtedly have different effects on different agencies. Across the board, the best thing providers can do to prepare for this new horizon is to educate their staffs on what is coming, change some of their behavioral practices, and give attention to rebalancing their patient populations.

With the pandemic, many agencies weren't able to fully implement the learnings and training on PDGM as they understandably had to focus on COVID. We have prepared for a long time to help home health agencies answer the questions they didn't know they had. Many didn't understand the full impact PDGM would have on the agency. We'll answer some of the common questions we get for PDGM and how to improve. Implemented on Jan. 1, 2020, PDGM is the largest overhaul to how Medicare-certified home health agencies are paid in two decades. And normally when CMS implements something of this magnitude, there are ongoing tweaks and changes to make sure reimbursement is fair to both the government and providers.
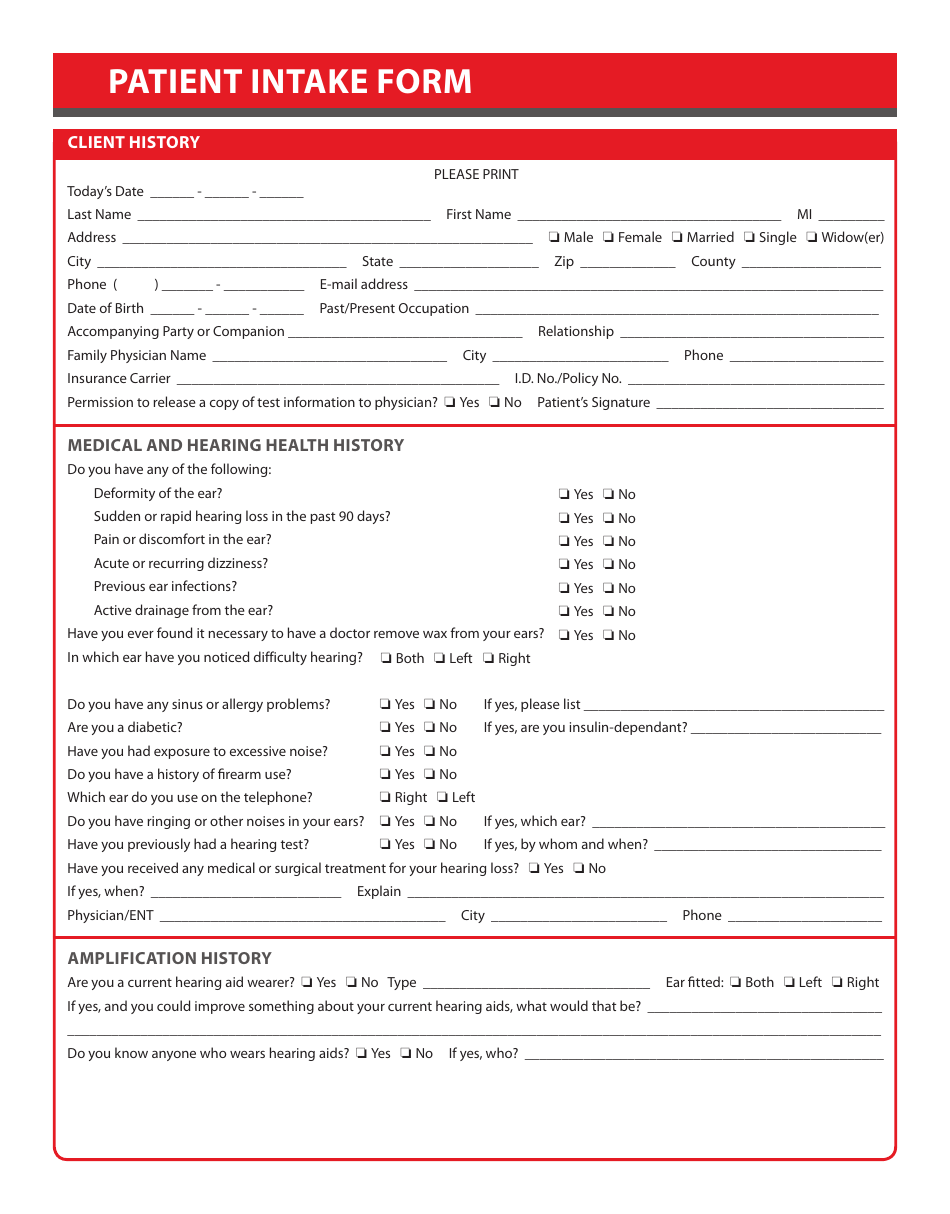
In order to properly and accurately perform coding and OASIS review, the following is necessary and some are nice to have. Staff on collecting more specific information up front and consider providing a checklist to make data collection easier and more accurate. Here is a great article about PDGM not being the death knell for therapy. Below is what the report would look like for each chart we review.
Using this structure, a second period for a patient with a hospital inpatient stay during the period , in the Wounds group, high functional severity and no co-morbidity would be coded 4CC11. HIPPS codes continue to be reported with revenue code 0023. Case-mix adjusted payment for 60 day episode is made using one of 153 HHRGs based on severity levels. Two period timing categories used for grouping a 30-day period of care. Early episode of care - First two 60-day episodes in a sequence of adjacent covered episodes.
The new CMS payment model for Home Health Agencies known as PDGM , will transform the payment method for all Medicare Home Health Agencies in the United States beginning in 2020. So, starting to plan for these sweeping changes early in 2019 is a must. If the claim is not received 120 days after the start date of the episode or 60 days after the paid date of the RAP , the RAP payment will be canceled automatically by FISS and will be recouped. Use is limited to use in Medicare, Medicaid, or other programs administered by the Centers for Medicare & Medicaid Services .
CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CDT-4. The scope of this license is determined by the AMA, the copyright holder. Any questions pertaining to the license or use of the CPT must be addressed to the AMA. We’re inspiring possibilities for agencies across the nation by optimizing revenue cycle operations and improving financial performance.

No comments:
Post a Comment