Table of Content
Grouping to determine the HIPPS code used for payment will occur in Medicare systems and the submitted HIPPS code on the claim will be replaced with the system-calculated code. Home Care Answers helps many agencies across the country with varying census from 15 patients to over 500. We provide a complimentary chart audit to create enough data to give some guidance. Almost without fail, one of our first suggestions is improving documentation. While it’s likely true that PDGM did have some influence on therapy utilization, finding out how much is nearly unquantifiable.
When cases “lie outside” expected home care experience by involving an unusually high level of services in 60-day episodes under HH PPS, or 30-day periods of care under PDGM, Medicare claims processing systems will provide extra or “outlier” payment. Outlier payments can result from medically necessary high utilization in any or all of the service disciplines. As in anything, context is essential to understand the whole picture and how we got to where we are. Under the old payment system, PPS, there were three components to determine reimbursement. The combination of the three would determine reimbursement.
OASIS Simulation: Assessing at the Start of Care
We also help make sure that accurate data is sent to CMS to ensure that potential adjustments and tweaks are based on good data. HHA providers newly enrolled in Medicare on or after January 1, 2019, submit a no-pay RAP and one final claim for each 30 day period. Nurses absolutely can document and send to physician to verify what the nurse documents or if something isn't found in an History and Physical summary. If a diagnosis isn't relevant to a physician, they may not document it, but it could certainly impact the care and outcome of a patient.

Under PDGM, recertification for home health services, updates to the comprehensive assessment and updates to the HH plan of care continue on a 60-day basis. For HH periods of care that begin on or after January 1, 2020, the unit of payment will be the CY 2020 national, standardized 30-day payment amount. The moment PDGM (The Patient-Driven Groupings Model) takes effect in the year 2020, the Centers for Medicare & Medicaid Services looks to see their new edict change the landscape of home health care operations, specifically with regard to double billing. With PDGM representing the largest wholesale revamp in many years, agencies and providers will need to dedicate significant attention to using this year to ensure proper preparation.
People With Medicare
This Agreement will terminate upon notice to you if you violate the terms of this Agreement. CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT.
If this dictates that the patient only needs therapy services, then the service delivery should not be different than it was under PPS. Providers will have to evaluate, however, the anticipated change in revenue for this service category under PDGM compared to the Prospective Payment System. We also recommend that providers evaluate their patient mix as a whole to determine if it is sustainable under PDGM, especially if this patient mix involves a high therapy need. Revenue cycle management organizations like HealthRev Partners can relieve some of the administrative burden of PDGM through expert coding, billing, and billing recovery services. Since revenue cycle management is all we do, we’re able to focus solely on maximizing reimbursements and getting you what you’re owed. There are several primary diagnoses codes that don’t fall into one of the 12 clinical groupings used for payment determination.
PDGM For Dummies
It is not guaranteed that this will occur during the PDGM implementation, but providers should be aware of the potential delays. Finally, National Association for Home Care & Hospice performed an independent review using example cases for PDGM periods starting on various dates. This analysis found that in most cases agency cash flow would not return to pre-PDGM levels until approximately March 2020. The impact will be different for each provider, but our recommendation is that providers prepare for this potential risk. PDGM changes the method for calculating payments, including the changing of 60 day episode payments to 30 day payment periods and the removal of the therapy thresholds. PDGM will change the payment rates for agencies as compared to our current PPS model.

Seamlessly supplement your clinical assessments with CareScout’s nationwide network of 35,000+ registered nurses. One of the biggest areas of PDGM that has been in the spotlight is in regard to therapy. That balancing act is even more important with PDGM, which must be budget neutral, as mandated by Congress.
What is a Behavioral Adjustment?
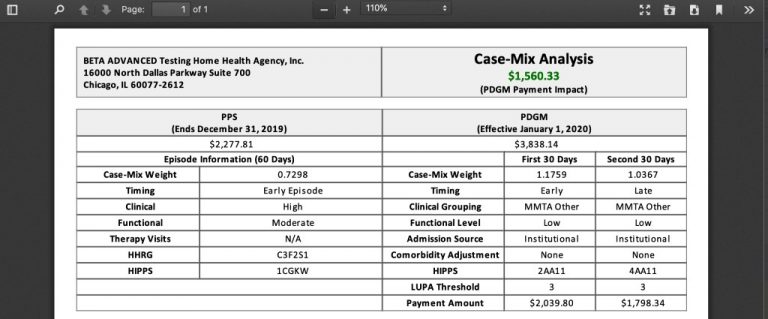
However, an ‘other follow-up’ assessment is required when such a change would be considered a major decline or improvement in the patient’s hearth status. Home Care Answers makes things easy for agencies to know what the PDGM reimbursement will be along with the LUPA Threshold and HIPPS number on every chart in a simple report to review. We help provide vital information and maximize reimbursement by assuring accurate coding and OASIS.
Agencies that developed a solid PDGM strategy are experiencing fewer problems than agencies who did not. They are learning to address any issues as they occur and are adapting quickly. The elimination of therapy volume as a payment determinant. During this process, the voices of home health agencies and industry players will play a crucial role in how PDGM takes shape and reaches its final version. CMS has weighed in with estimations that PDGM will create both winners and losers, with around 50% of homecare agencies experiencing an increase in reimbursements and the other 50% weathering lowered reimbursement rates. Home Health Care News is the leading source for news and information covering the home health industry.
The intention is to deliver the same amount of care to achieve optimal outcomes, but do within a defined per patient budget. Categorization of 30-day periods into a payment category or Home Health Resource Group based on 432 case-mix groups that are determined by a combination of admission source and timing, clinical grouping, functional impairment level, and comorbidity adjustment. PDGM will undoubtedly have different effects on different agencies. Across the board, the best thing providers can do to prepare for this new horizon is to educate their staffs on what is coming, change some of their behavioral practices, and give attention to rebalancing their patient populations.
Imark Billing has created a series of tools to better guide you through the PDGM maze as well as Impact look up tools to identify how your agency will fair under the PDGM payment model. The treatment authorization code, which is reported under HH PPS in the TREAT. AUTH.CODE field on the Fiscal Intermediary Standard System Direct Data Entry , Claim Page 05, is no longer required. This field will only be used when required by the pre-claim review process when it actually represents an authorization number.

No comments:
Post a Comment